- Home
- ::
- Vitamin Toxicity: The Two Vitamins You Must Watch

Vitamin Toxicity: The Two Vitamins You Must Watch
Vitamin A & D Intake Calculator
How to Use This Calculator
Enter your daily intake of vitamin A and D from supplements and fortified foods. This tool compares your intake against safe upper limits (UL) established by health authorities.
Your intake:
Note: This tool is informational only. Consult a healthcare provider for personalized advice.
When you hear "vitamins are good for you," it’s easy to forget that too much can be dangerous. Among the 13 essential vitamins, two stand out for their high toxicity risk when taken in excess: vitamin A and vitamin D. Understanding why these two are troublemakers, how much is too much, and what symptoms to watch for can keep you safe while you reap the benefits of supplementation.
What Makes Vitamin A and Vitamin D Different from the Rest?
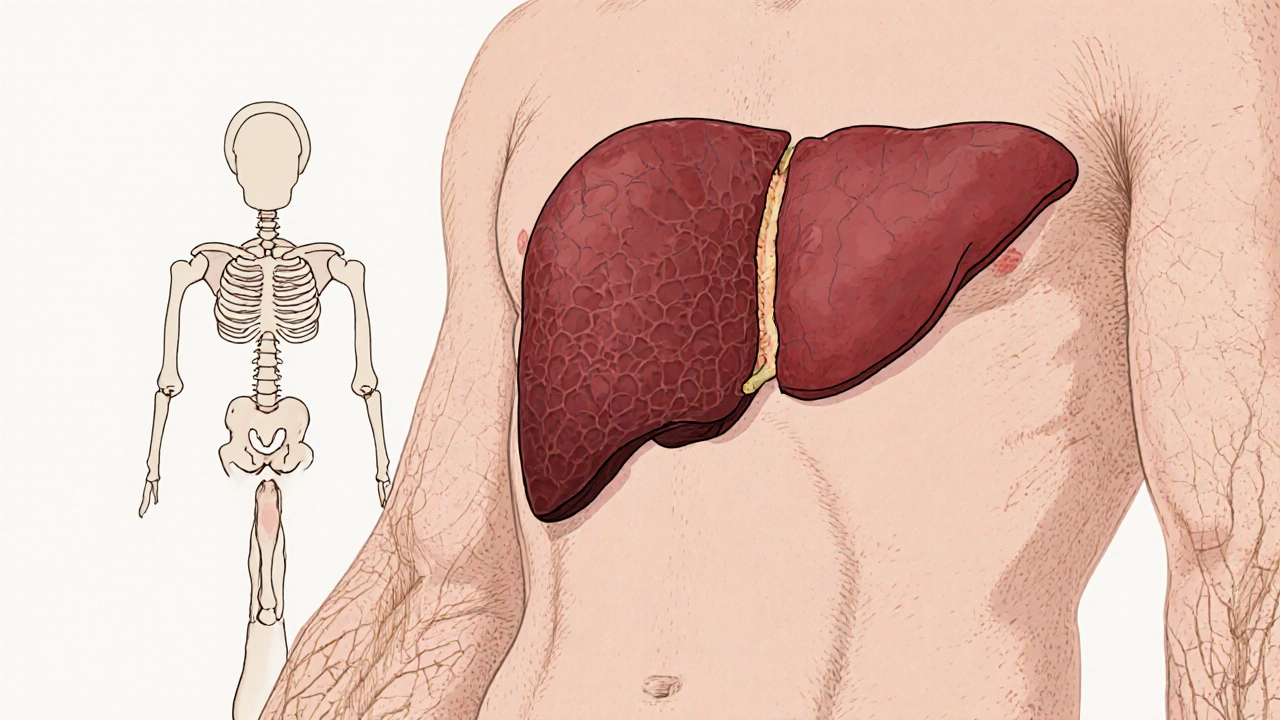
Both belong to the fat‑soluble vitamins a group of vitamins (A, D, E, K) that dissolve in fats and are stored in the liver and fatty tissues. Unlike water‑soluble vitamins (like B‑complex and C) that the body flushes out quickly, fat‑soluble vitamins linger, building up over time. This storage ability turns a good thing into a problem if you consistently exceed the recommended intake.
Vitamin A: The Double‑Edged Warrior
Vitamin A a fat‑soluble vitamin essential for vision, immune function, and cellular growth exists in two primary forms: preformed retinol (found in animal sources) and provitamin A carotenoids (found in plant foods). The toxicity issue centers on preformed retinol because the body converts carotenoids to retinol only as needed.
- Upper intake limit (UL): 3,000 µg retinol activity equivalents (RAE) per day for adults (≈10,000 IU).
- Common sources of excess: high‑dose prescription supplements, liver‑rich foods (e.g., beef liver), and certain multivitamins marketed for skin health.
- Symptoms of acute toxicity: nausea, headache, dizziness, blurred vision.
- Chronic toxicity signs: dry, rough skin, hair loss, bone pain, and in extreme cases, liver damage and birth defects.
One study of 2,500 patients in the U.K. found that 4% of those taking >5,000 IU daily for more than six months developed elevated liver enzymes, a clear marker of hepatic stress.
Vitamin D: The Sunshine Vitamin Gone Rogue
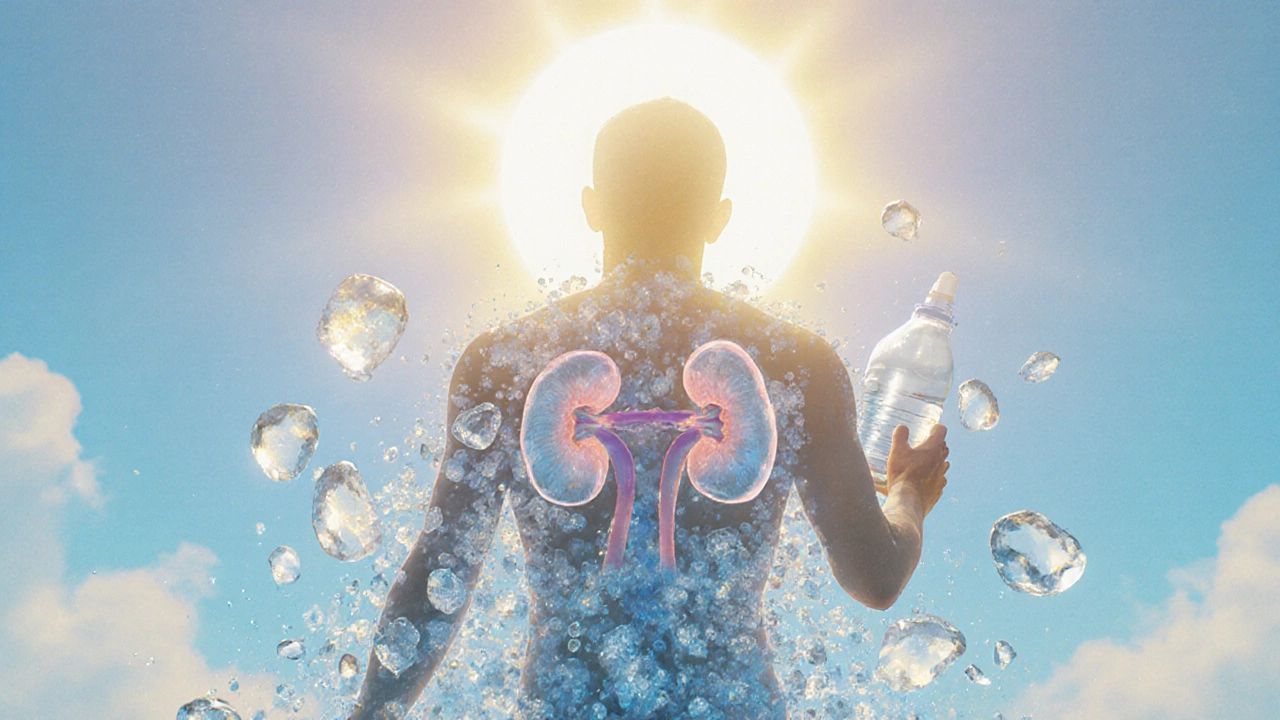
Vitamin D a fat‑soluble vitamin that regulates calcium and phosphorus absorption, crucial for bone health and immune function exists mainly as D2 (ergocalciferol) from plant sources and D3 (cholecalciferol) from animal sources and skin synthesis. The modern push for higher vitamin D levels, combined with easy‑access supplements, has led to a rise in overdoses.
- Upper intake limit (UL): 100 µg (4,000 IU) per day for adults.
- Typical overdose sources: mega‑dose vitamin D tablets (often 5,000-10,000 IU), fortified foods, and misuse of prescription forms for osteoporosis.
- Acute toxicity signs: nausea, vomiting, weakness, and excessive thirst.
- Chronic toxicity outcomes: hypercalcemia, kidney stones, calcification of soft tissues, and cardiovascular complications.
Data from a 2023 NHS audit of 1,800 patients on high‑dose vitamin D showed that 7% developed hypercalcemia, with 2% requiring hospitalization for renal complications.
Why These Two Vitamins Pose the Greatest Risk
The convergence of three factors makes vitamin A and vitamin D the primary culprits:
- Fat solubility and storage: Both accumulate in liver and adipose tissue, leading to a slow but steady buildup.
- Wide availability: Over‑the‑counter supplements, fortified foods, and prescription products make it easy to exceed safe levels.
- Therapeutic hype: Media coverage touting “immune‑boosting” or “anti‑aging” benefits encourages high‑dose use without medical supervision.
Other vitamins, like C or the B‑complex, are water‑soluble and usually excreted quickly, so toxicity is rare even at high intakes.
How to Spot Toxicity Early
Because symptoms overlap with many common ailments, you need a systematic approach:
- Track supplement intake: Keep a daily log of all vitamins, doses, and brand names.
- Watch lab markers: Liver function tests (ALT, AST) for vitamin A; serum calcium and 25‑hydroxy‑vitamin D levels for vitamin D.
- Listen to your body: Persistent skin issues, unexplained bone pain, or frequent thirst could signal excess.
If you suspect toxicity, stop the supplement immediately and consult a healthcare professional. Blood tests can confirm whether levels are above the safe range.
Safe Supplementation Strategies
Here are practical steps to enjoy the benefits without the risk:
- Know your baseline: Get a blood test before starting any high‑dose vitamin regimen.
- Follow recommended dietary allowances (RDA): For most adults, 700‑900 µg RAE of vitamin A and 15‑20 µg (600‑800 IU) of vitamin D are sufficient.
- RDA references come from the UK's NHS and the Institute of Medicine.
- Prefer food sources over pills: A serving of salmon provides ~450 IU of vitamin D, while a cup of carrots offers ~8,000 µg RAE of provitamin A carotenoids, which the body regulates.
- Beware of “mega‑dose” marketing: Products promising 10,000 IU of vitamin D or more should be taken only under medical supervision.
- Review all medications: Some prescription drugs (e.g., orlistat) affect fat absorption and can alter vitamin storage.
Comparison Table: Vitamin A vs. Vitamin D Toxicity
| Aspect | Vitamin A | Vitamin D |
|---|---|---|
| Primary toxic form | Preformed retinol (retinyl esters) | Cholecalciferol (vitamin D3) and ergocalciferol (vitamin D2) |
| Upper intake limit (UL) | 3,000 µg RAE (≈10,000 IU) | 100 µg (4,000 IU) |
| Typical overdose sources | High‑dose supplements, liver pâté, certain skin‑care pills | Mega‑dose tablets, fortified milks, prescription osteoporosis meds |
| Acute toxicity symptoms | Nausea, headache, blurred vision | Nausea, vomiting, excessive thirst |
| Chronic toxicity signs | Dry skin, bone pain, liver enlargement, birth defects | Hypercalcemia, kidney stones, soft‑tissue calcification |
| Key organ affected | Liver (hepatotoxicity) | Kidneys (nephrocalcinosis) and cardiovascular system |
Special Populations: Who Should Be Extra Cautious?
Pregnant women, children, and people with liver or kidney disease face higher risks. For example, excess vitamin A during pregnancy is linked to neural tube defects, while those with chronic kidney disease can’t excrete excess calcium from vitamin D, amplifying the danger.
Guidelines from the Royal College of Obstetricians and Gynaecologists advise pregnant women to stay under 2,500 µg RAE of vitamin A and avoid high‑dose vitamin D unless prescribed.
What to Do If You Overdose
Immediate steps can mitigate damage:
- Stop the source: Discontinue the supplement or fortified product.
- Hydrate: For vitamin D excess, increased water intake helps flush calcium.
- Medical evaluation: Blood tests for liver enzymes (ALT, AST) and serum calcium.
- Treatment options:
- Vitamin A toxicity: corticosteroids may reduce inflammation; severe cases need liver support.
- Vitamin D toxicity: bisphosphonates or calcitonin to lower calcium levels, and IV fluids.
Most mild cases resolve with cessation and monitoring, but severe hypercalcemia can be life‑threatening.
Bottom Line: Balance Is Key
Vitamins are vital, but unlike calories, they don’t have a “burn‑off” mechanism once stored. Vitamin A and vitamin D carry the highest toxicity potential because they’re fat‑soluble, widely available, and often over‑promoted. By tracking intake, testing levels, and respecting upper limits, you can enjoy their health benefits without risking liver damage or calcium overload.
Frequently Asked Questions
Can I get vitamin A toxicity from eating carrots?
No. Carrots contain beta‑carotene, a provitamin A that the body converts to retinol only as needed. Toxicity mainly comes from pre‑formed retinol found in liver, high‑dose supplements, or fortified foods.
What blood test confirms vitamin D overdose?
A serum 25‑hydroxy‑vitamin D level above 250nmol/L (100ng/mL) combined with raised calcium (>2.6mmol/L) signals toxicity.
How quickly do symptoms appear after an overdose?
Acute symptoms can emerge within hours to a few days, especially with very high single doses. Chronic symptoms develop over weeks or months of steady excess.
Are there safe ways to take high‑dose vitamin D for deficiency?
Yes, but only under medical supervision. A doctor may prescribe 10,000IU daily for a short period, followed by regular monitoring of blood calcium and vitamin D levels.
What should I do if I notice early signs of toxicity?
Stop the supplement immediately, schedule a lab test, and consult a healthcare provider. Early intervention usually prevents permanent organ damage.

 Health and Wellness
Health and Wellness





Write a comment